
After birth, this same sequence of events (matrix mineralization, death of chondrocytes, invasion of blood vessels from the periosteum, and seeding with osteogenic cells that become osteoblasts) occurs in the epiphyseal regions, and each of these centers of activity is referred to as a secondary ossification center ( e). By the time the fetal skeleton is fully formed, cartilage only remains at the joint surface as articular cartilage and between the diaphysis and epiphysis as the epiphyseal plate, the latter of which is responsible for the longitudinal growth of bones. While these deep changes are occurring, chondrocytes and cartilage continue to grow at the ends of the bone (the future epiphyses), which increases the bone’s length at the same time bone is replacing cartilage in the diaphyses. By the second or third month of fetal life, bone cell development and ossification ramps up and creates the primary ossification center, a region deep in the periosteal collar where ossification begins ( c). Here, the osteoblasts form a periosteal collar of compact bone around the cartilage of the diaphysis. This penetration initiates the transformation of the perichondrium into the bone-producing periosteum. These enlarging spaces eventually combine to become the medullary cavity.Īs the cartilage grows, capillaries penetrate it. Blood vessels invade the resulting spaces, not only enlarging the cavities but also carrying osteogenic cells with them, many of which will become osteoblasts. This results in their death and the disintegration of the surrounding cartilage. As the matrix calcifies, nutrients can no longer reach the chondrocytes. (f) Cartilage remains at epiphyseal (growth) plate and at joint surface as articular cartilage.Īs more matrix is produced, the chondrocytes in the center of the cartilaginous model grow in size. (e) Secondary ossification centers develop. (d) Cartilage and chondrocytes continue to grow at ends of the bone. Perichondrium transforms into periosteum. (b) The cartilage model of the future bony skeleton and the perichondrium form. (a) Mesenchymal cells differentiate into chondrocytes.

The trabecular bone crowds nearby blood vessels, which eventually condense into red marrow ( d).Įndochondral ossification follows five steps. The periosteum then creates a protective layer of compact bone superficial to the trabecular bone. Osteoid (unmineralized bone matrix) secreted around the capillaries results in a trabecular matrix, while osteoblasts on the surface of the spongy bone become the periosteum ( c). As osteoblasts transform into osteocytes, osteogenic cells in the surrounding connective tissue differentiate into new osteoblasts. Once entrapped, the osteoblasts become osteocytes ( b). The osteoblasts secrete osteoid, uncalcified matrix, which calcifies (hardens) within a few days as mineral salts are deposited on it, thereby entrapping the osteoblasts within.
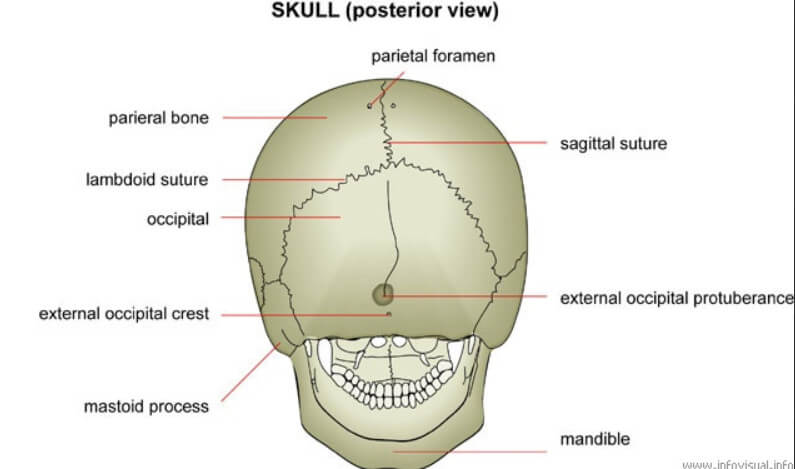
Although they will ultimately be spread out by the formation of bone tissue, early osteoblasts appear in a cluster called an ossification center. Some of these cells will differentiate into capillaries, while others will become osteogenic cells and then osteoblasts. The process begins when mesenchymal cells in the embryonic skeleton gather together and begin to differentiate into specialized cells ( a). The flat bones of the face, most of the cranial bones, and the clavicles (collarbones) are formed via intramembranous ossification. Some additional cartilage will be replaced throughout childhood, and some cartilage remains in the adult skeleton.ĭuring intramembranous ossification, compact and spongy bone develops directly from sheets of mesenchymal (undifferentiated) connective tissue.

By the time a fetus is born, most of the cartilage has been replaced with bone. Throughout fetal development and into childhood growth and development, bone forms on the cartilaginous matrix. This is why damaged cartilage does not repair itself as readily as most tissues do. All of these functions are carried on by diffusion through the matrix. Unlike most connective tissues, cartilage is avascular, meaning that it has no blood vessels supplying nutrients and removing metabolic wastes. As the matrix surrounds and isolates chondroblasts, they are called chondrocytes. This framework is a flexible, semi-solid matrix produced by chondroblasts and consists of hyaluronic acid, chondroitin sulfate, collagen fibers, and water. During fetal development, a framework is laid down that determines where bones will form. For skeletal development, the most common template is cartilage. Bone is a replacement tissue that is, it uses a model tissue on which to lay down its mineral matrix.


 0 kommentar(er)
0 kommentar(er)
